Planning the Health Workforce of the Future: What Can We Learn from Norway?
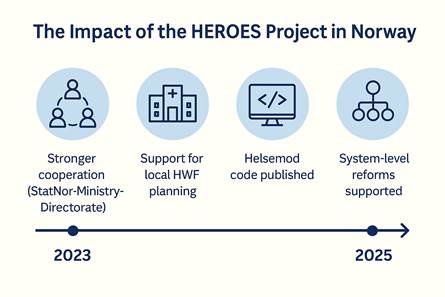
6th HEROES Community of Practice Meeting
Date: March 7, 2025 | Host: Norwegian Directorate of Health
The session introduced participants to Helsemod, Norway’s national health workforce (HWF) projection model, with a focus on its potential use beyond national borders.
Guests: Helen Brandstorp, Division Director of Municipal Health Services and Emergency Preparedness Division, Jia Zhiyang, Senior Researcher at Statistics Norway and Erik Sirnes, Senior Adviser at the Norwegian Ministry of Health and Care Services.
Europe’s healthcare systems are grappling with a common reality: an ageing population, changing expectations and a looming shortage of skilled professionals. In this context, 6th HEROES Community of Practice (CoP) meeting, organised by the Norwegian Directorate of Health, provided a timely and compelling insight into how one country is tackling these challenges – and how others can follow suit.
Titled “An introduction to the Norwegian HWF planning and forecasting model – Can it be used in your country as well?”, the online session brought together public officials, researchers, and policymakers from across Europe to explore how forecasting tools can drive smarter health workforce (HWF) planning.
“Healthcare workers are the backbone of our system”
Opening the session, Dr. Helen Brandstorp, Division Director for Municipal Health Services and Emergency Preparedness, provided a frank overview of the current situation in Norway:
“Like many other European countries, we are facing an increasingly old population, not enough people, and not enough health personnel in the coming years. It is of critical importance that the healthcare sector has sufficient and competent staff.”
She emphasized that Norway, with its 357 municipalities, many of them small and rural, requires not only national-level planning, but also support for local-level capacity building and forecasting. She added that participation in the HEROES Joint Action had already made a visible difference:
“Many of these activities would not have happened without the joint action, and we’re grateful for the boost it has given to our work.”
Transparent, flexible, and simple: The Helsemod model
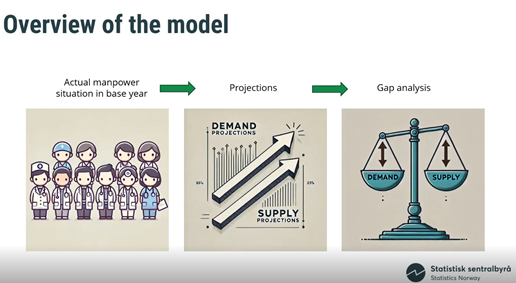
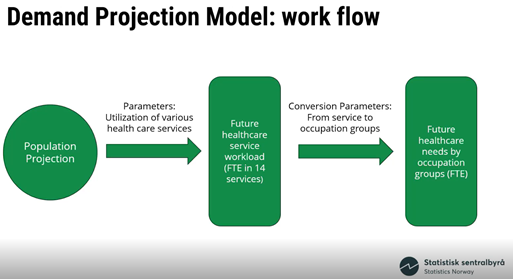
The core of the session was an in-depth presentation by Jia Zhiyang, Senior Researcher at Statistics Norway, who walked participants through the workings of Helsemod, the country’s national HWF forecasting model.
Developed originally in the 1990s and continuously improved, Helsemod projects both supply and demand for 14 healthcare professions. It uses real administrative data to estimate labour market flows and full-time equivalents (FTEs), including inflows (graduates, immigration), outflows (retirement, migration), and part-time work patterns.
What sets the model apart is its transparency and simplicity:
“We don’t want a black box. If policymakers can’t understand the model, they won’t trust it. We deliberately kept it clear and reproducible,” Jia explained.
The model also allows for scenario-based planning. Users can test the impact of various policy options, such as increasing training intake, delaying retirement, or adjusting task distribution across professions. It’s already being used to inform decisions at multiple levels of government – and now, it’s being prepared for open publication on GitHub, to support international use and collaboration.
Future Directions and Key Challenges
While the model functions well, experts from Statistics Norway acknowledged the need for updates to keep it relevant. Future improvements may include:
- Enhancing accessibility and user-friendliness
- Expanding the model’s capabilities to regional and local levels
- Integrating qualitative data for richer scenario-building
These enhancements would allow the model to support an even broader range of stakeholders and planning needs.
In general, there are not many significant challenges associated with this area. With regard to the Helsemod model, it is considered sufficient, but would benefit from updates to make it more current and accessible. Enhancing its capabilities to handle a broader range of scenarios and integrating qualitative data would also be advantageous. One of the main challenges currently being addressed is the improvement of projections at sub-national levels, as the model currently operates primarily at the national level. This is regarded as the most significant challenge at present.
“A model is only useful if it influences policy”
While forecasting models are often seen as abstract tools, Erik Sirnes, Senior Adviser at the Norwegian Ministry of Health and Care Services, made it clear:
“This model is not just academic – it’s actively shaping real decisions.”
Erik outlined how Helsemod’s outputs played a central role in:
- A recent Norwegian official report on health workforce needs (led by an independent commission)
- The development of the government’s White Paper on National Health and Coordination
- Strategic discussions about education capacities, task shifting, and care integration
Importantly, the ministry recognized that the projected gaps cannot be closed by increasing supply alone:
“It’s not possible to meet the challenges by simply adding more people. We must work on the demand side too — improve efficiency, rethink service delivery, and prioritize where needed.”
From scenario to strategy: What happens when we change the assumptions?
The session also delved into how the model handles “what-if” scenarios – such as increased immigration, faster digitalisation, or changing patient needs. One critical insight came from backcasting: applying today’s standards to the 1970s population. The result? Health workforce demand would have doubled.
This revealed a powerful but sobering fact:
“Only half of the increase in workforce since the 1970s is due to population growth and ageing. The other half comes from higher expectations, new rights, and increased care standards.”
That trajectory is unlikely to be sustainable. As Erik pointed out:
“The problem isn’t just money. It’s the lack of available people. And other countries face the same challenge. Relying on international recruitment isn’t a viable – or ethical – long-term strategy.”
Emerging lessons and future ambitions
The HEROES meeting underscored several broader takeaways for the European HWF community:
- Scenario modelling is not optional – it is essential to prepare for uncertainty and guide proactive planning.
- Models must be accessible – not only technically, but politically and culturally.
- Cross-level cooperation matters – aligning national models with regional realities increases their relevance.
- Transparency builds trust – publishing code and assumptions encourages learning and quality improvement.
- Planning ≠ Forecasting – closing the gap requires not just insight, but action, prioritization, and reform.
Jia summed it up well:
“We’ve benefited immensely from the HEROES project. It has given us the opportunity to reflect, to improve, and to connect. We hope to inspire others – and learn in return.”
From Norway to Europe – and beyond
Helsemod may have been designed for a Norwegian context, but the principles behind it – clarity, usability, adaptability – are universally relevant. As countries across Europe rethink how they plan their health workforce, tools like this offer a compelling starting point.
Whether your country needs a model or a method, a dataset or a dialogue – the message from Norway is clear: start now, stay transparent, and use what you have to shape what you need.
Topic in 5 Words:
Forecasting – Policy – Collaboration – Transparency – Future